Working With Bunions
Overview
 A bunion (also called Hallux Valgus) is a painful swelling caused by deformity of the big toe. As this swelling is caused by a bone it can be very unforgiving in shoes, which can rub on it causing pain, particularly formal foot shoes or high heels. Arthritis, or wearing tight or ill-fitting shoes over a period of many years, may increase the risk of bunions. However, they can have other causes. Bunions are more common in women and sometimes run in families.
A bunion (also called Hallux Valgus) is a painful swelling caused by deformity of the big toe. As this swelling is caused by a bone it can be very unforgiving in shoes, which can rub on it causing pain, particularly formal foot shoes or high heels. Arthritis, or wearing tight or ill-fitting shoes over a period of many years, may increase the risk of bunions. However, they can have other causes. Bunions are more common in women and sometimes run in families.
Causes
You are usually born with a foot type that leads to bunion formation. Flat feet with increased flexibility are most likely to form bunions. Abnormal mechanics increase the bunion formation over time. Other causes of bunions include osteoarthritis, gout, rheumatoid arthritis, trauma, and neurovascular disease.
Symptoms
The major symptom of bunions is a hard bump on the outside edge of the foot or at the base of the big toe. Redness, pain and swelling surrounding or at the MTP joint can also occur.
Diagnosis
Before examining your foot, the doctor will ask you about the types of shoes you wear and how often you wear them. He or she also will ask if anyone else in your family has had bunions or if you have had any previous injury to the foot. In most cases, your doctor can diagnose a bunion just by examining your foot. During this exam, you will be asked to move your big toe up and down to see if you can move it as much as you should be able to. The doctor also will look for signs of redness and swelling and ask if the area is painful. Your doctor may want to order X-rays of the foot to check for other causes of pain, to determine whether there is significant arthritis and to see if the bones are aligned properly.
Non Surgical Treatment
Follow the advice given by a Podiatrist. Use felt pads to help keep pressure off the painful area of the bunions. Wear shoes that are wide and deep to accomodate the bunions. Fitting of footwear is very important. Avoid the use of high heel shoes. Use exercises to keep the joint mobile. Night splints may help with the bunion symptoms. The aim of these are to hold the toe in a more correct position. Padding or foam between the big toe and the second toe is sometimes recommended, it should, generally, not be recommended as the big toe is usually so strong it just further 'squeezes' the lesser toes and can lead to problems between these toes. The padding between the two toes will not straighten the big toe. However, sometimes the padding may be needed to help with symptoms that originate inside the joint if the bunion is painful. 
Surgical Treatment
Some sufferers choose to have the bunion surgically removed. This should always be a last resort as all surgeries carry risks. There are several types of surgical procedures to remove bunions and before deciding, you should speak to your surgeon at length about the facts and risks associated with surgery, including the recovery time and success rate of the operation to be done. Please note that if you have a surgical procedure and then return to your high heels and narrow-toed shoes, the bunion is likely to reoccur.
Prevention
To help prevent bunions, select your style and size of shoes wisely. Choose shoes with a wide toe area and a half-inch of space between the tip of your longest toe and the end of the shoe. Shoes also should conform to the shape of your feet without causing too much pressure.
Over-Pronation Of The Foot What Are The Treatments
Pronation is the natural way that our feet absorb shock: when our feet strike the ground the arches flex down and in to disperse the impact. Everyone pronates! Contrary to popular misconception it is healthy and normal. The problem begins when one or both of our feet pronate too much. When the arches flex too far inward or stay collapsed for too long pronation is considered excessive. We call this overpronation. The amount of overpronation can vary from mild to severe. In severe overpronation the feet and ankles can rotate too far inward just during standing.

Causes
During our development, the muscles, ligaments, and other soft tissue structures that hold our bones together at the joints become looser than normal. When the bones are not held tightly in place, the joints are not aligned properly, and the foot gradually turns outward at the ankle, causing the inner ankle bone to appear more prominent. The foot moves in this direction because it is the path of least resistance. It is more difficult for the foot to move in the opposite direction (this is called supination). As we develop, the muscles and ligaments accommodate to this abnormal alignment. By the time growth is complete, the pronated foot is: abnormally flexible, flat, and its outer border appears raised so that as you step down you do not come down equally across the entire foot; instead, you come down mostly on the inner border of the foot. Normal aging will produce further laxity of our muscles that causes the pronation to become gradually worse.
Symptoms
Because overpronation affects the entire lower leg, many injuries and conditions may develop and eventually cause problems not only in the leg and foot, but also the knee, hips and lower back. Pain often begins in the arch of the foot or the ankle. Blisters may develop on the instep, or on the inside edge of the heels. As overpronation continues and problems develop, pain will be felt elsewhere, depending on the injury.
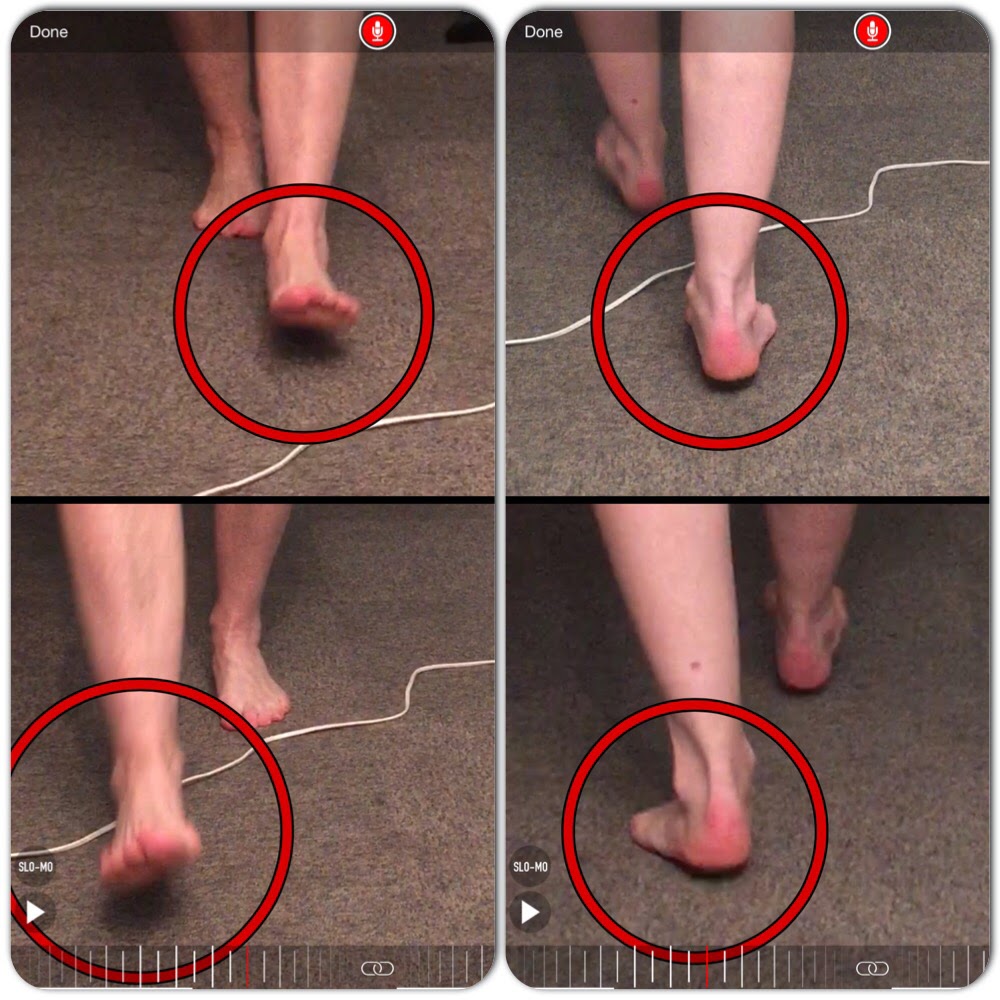
Diagnosis
Firstly, look at your feet in standing, have you got a clear arch on the inside of the foot? If there is not an arch and the innermost part of the sole touches the floor, then your feet are over-pronated. Secondly, look at your running shoes. If they are worn on the inside of the sole in particular, then pronation may be a problem for you. Thirdly, try the wet foot test. Wet your feet and walk along a section of paving and look at the footprints you leave. A normal foot will leave a print of the heel, connected to the forefoot by a strip approximately half the width of the foot on the outside of the sole. If you?re feet are pronated there may be little distinction between the rear and forefoot, shown opposite. The best way to determine if you over pronate is to visit a podiatrist or similar who can do a full gait analysis on a treadmill or using forceplates measuring exactly the forces and angles of the foot whilst running. It is not only the amount of over pronation which is important but the timing of it during the gait cycle as well that needs to be assessed.
Non Surgical Treatment
Get a gait analysis of your running style, this will highlight if you overpronate, oversupinate or have a neutral gait. Most podiatrists, physio's and sports therapists will offer this service, as do some specialist sports shops. Find a clinic. If you overpronate, get orthotics with extra medial support. Many running shoes have a harder material on the inside of the midsole (the thick hard foam part of the running shoe). This means the inside of the shoe will be compressed less under load and support the inside of the foot preventing it from rolling in or flattening. For people with considerable overpronation, another option is to have an orthotic device fitted. Orthotic insoles come in many types and prices. Some are pre-molded and can be bought off the shelf. These are ok for the majority of problem feet. However some cases may require specially casted orthotics from a relevant sports injury therapist or podiatrist.
Surgical Treatment
Depending on the severity of your condition, your surgeon may recommend one or more treatment options. Ultimately, however, it's YOUR decision as to which makes the most sense to you. There are many resources available online and elsewhere for you to research the various options and make an informed decision.
What Are The Causes Of Calcaneal Apophysitis?
Unlike adults, heel pain is very uncommon in children. When children do experience heel pain, it is highly likely to be caused by a disturbance to the growth plate in the backof the heel bone (calcaneus), where the Achilles tendon attaches to the heel. This disturbance is known as Sever?s disease or calcaneal apophysitis (inflammation of the growth plate). Sever?s disease is most common between the ages of 10 and 14 years, and it is one of several different ?osteochondroses? that may occur in other parts of the body, such as at the knee, such as Osgood-Schlatters Disease. This condition occurs in children because they are still growing and their bodies harbor many ?growth plates?. A growth plate, also called an epiphyseal plate, is an area at the end of a developing bone where cartilage cells change over time into bone cells. As this occurs, the growth plates expand and unite, which is how bones grow.
Causes
Your child?s heel bone keeps forming new bone until the late teens. The new bone is weak and can be damaged by running or pounding on hard surfaces, like during a basketball game. The new bone may also be irritated by shoes with poor padding in the heels or poor arch supports.
Symptoms
The symptoms of Sever?s Disease may vary but usually include generalised pain and discomfort around the back of the heel. Can be one sided or both sides. Starts after child starts a new sport season. May cause child to limp due to pain. Increases with weight bearing activity. Heel becomes red and can be swollen. X-rays are usually inconclusive and simply show the growth plate.
Diagnosis
A doctor can usually tell that a child has Sever's disease based on the symptoms reported. To confirm the diagnosis, the doctor will probably examine the heels and ask about the child's activity level and participation in sports. The doctor might also use the squeeze test, squeezing the back part of the heel from both sides at the same time to see if doing so causes pain. The doctor might also ask the child to stand on tiptoes to see if that position causes pain. Although imaging tests such as X-rays generally are not that helpful in diagnosing Sever's disease, some doctors order them to rule out other problems, such as fractures. Sever's disease cannot be seen on an X-ray.
Non Surgical Treatment
Occasionally, an orthotic may need to be prescribed for temporary or long-term correction of their foot biomechanics (eg flat feet or high arches). During the acute phase of Sever's disease a small heel rise or shock-absorbing heel cup placed under the heel pad of your child's foot may help to ease the symptoms. Your podiatrist or physiotherapist can assess your child's arch and guide you in the best management of your child's condition. We recommend that your child should never go barefooted during the painful stages of Sever's disease.
Recovery
If the child has a pronated foot, a flat or high arch, or another condition that increases the risk of Sever's disease, the doctor might recommend special shoe inserts, called orthotic devices, such as heel pads that cushion the heel as it strikes the ground, heel lifts that reduce strain on the Achilles tendon by raising the heel, arch supports that hold the heel in an ideal position. If a child is overweight or obese, the doctor will probably also recommend weight loss to decrease pressure on the heel. The risk of recurrence goes away on its own when foot growth is complete and the growth plate has fused to the rest of the heel bone, usually around age 15.
Which Are The Primary Causes Of Posterior Tibial Tendon Dysfunction (PTTD) ?
Overview
Adult flatfoot (adult acquired flatfoot) or posterior tibial tendon dysfunction (PTTD) is a common pathology presented to foot and ankle specialists. PTTD is characterized by a valgus (everted) hindfoot, flattening of the longitudinal arch of the foot (collapse) and abduction of the forefoot. This is a progressive deformity that begins flexible and can become rigid over time. The posterior tibial tendon (PT) is one of the main supporting structures of the foot arch. Changes within this tendon cause flattening of the foot. There are four stages of this deformity that begins flexible and progressives, with no treatment, to a rigid deformity and with time may involve the ankle joint. Patients usually present with pain in the foot or ankle stating the ?ankle? is rolling. It?s also common for patients to state they have difficulty walking barefoot. Pain is exacerbated after physical activities. Pain is usually isolated to the inside of the foot along the course of the PT tendon. 
Causes
There are numerous causes of acquired Adult Flatfoot, including, trauma, fracture, dislocation, tendon rupture/partial rupture or inflammation of the tendons, tarsal coalition, arthritis, neuroarthropathy and neurologic weakness. The most common cause of acquired Adult Flatfoot is due to overuse of a tendon on the inside of the ankle called the posterior tibial tendon. This is classed as - posterior tibial tendon dysfunction. What are the causes of Adult Acquired flat foot? Trauma, Fracture or dislocation. Tendon rupture, partial tear or inflammation. Tarsal Coalition. Arthritis. Neuroarthropathy. Neurological weakness.
Symptoms
Posterior tibial tendon insufficiency is divided into stages by most foot and ankle specialists. In stage I, there is pain along the posterior tibial tendon without deformity or collapse of the arch. The patient has the somewhat flat or normal-appearing foot they have always had. In stage II, deformity from the condition has started to occur, resulting in some collapse of the arch, which may or may not be noticeable. The patient may feel it as a weakness in the arch. Many patients initially present in stage II, as the ligament failure can occur at the same time as the tendon failure and therefore deformity can already be occurring as the tendon is becoming symptomatic. In stage III, the deformity has progressed to the extent where the foot becomes fixed (rigid) in its deformed position. Finally, in stage IV, deformity occurs at the ankle in addition to the deformity in the foot.
Diagnosis
Perform a structural assessment of the foot and ankle. Check the ankle for alignment and position. When it comes to patients with severe PTTD, the deltoid has failed, causing an instability of the ankle and possible valgus of the ankle. This is a rare and difficult problem to address. However, if one misses it, it can lead to dire consequences and potential surgical failure. Check the heel alignment and position of the heel both loaded and during varus/valgus stress. Compare range of motion of the heel to the normal contralateral limb. Check alignment of the midtarsal joint for collapse and lateral deviation. Noting the level of lateral deviation in comparison to the contralateral limb is critical for surgical planning. Check midfoot alignment of the naviculocuneiform joints and metatarsocuneiform joints both for sag and hypermobility.
Non surgical Treatment
Stage one deformities usually respond to conservative or non-surgical therapy such as anti-inflammatory medication, casting, functional orthotics or a foot ankle orthosis called a Richie Brace. If these modalities are unsuccessful surgery is warranted. 
Surgical Treatment
Many operations are available for the treatment of dysfunction of the posterior tibial tendon after a thorough program of non-operative treatment has failed. The type of operation that is selected is determined by the age, weight, and level of activity of the patient as well as the extent of the deformity. The clinical stages outlined previously are a useful guide to operative care (Table I). In general, the clinician should perform the least invasive procedure that will decrease pain and improve function. One should consider the effects of each procedure, particularly those of arthrodesis, on the function of the rest of the foot and ankle.
Cause Of Foot Pain In The Arch
Plantar fasciitis can be a real pain in the foot. Plantar fasciitis is the medical term for inflammation of the plantar fascia, which is the connective tissue that runs along the bottom of your foot. If you?ve ever had pain in the bottom of your foot with the first few steps out of bed in the morning, you?ve probably had some experience with this painful condition. In active populations, plantar fasciitis is often associated with overuse or a sudden change in activity, and temporarily easing off of activity can be part of the solution. In more sedentary populations, weight gain is usually a major contributor to plantar fasciitis and a weight-loss plan could be of benefit. Whether you?re active or sedentary, however, previous foot injuries, poor arch support, or tight muscles around the foot can all predispose you to plantar fasciitis.

Causes
Having low or no arches is normal for some people. In these cases, flat feet are usually inherited and the feet are fairly flexible. Occasionally, flat feet can be caused by an abnormality that develops in the womb, such as a problem with a joint or where two or more bones are fused together. This is known as tarsal coalition and results in the feet being flat and stiff. Flat feet that develop in later life can be caused by a condition that affects the joints, such as arthritis, or an injury to a muscle, tendon or joint in the foot.
Symptoms
Typically, the sufferer of plantar fasciitis experiences pain upon rising after sleep, particularly the first step out of bed. Such pain is tightly localized at the bony landmark on the anterior medial tubercle of the calcaneus. In some cases, pain may prevent the athlete from walking in a normal heel-toe gait, causing an irregular walk as means of compensation. Less common areas of pain include the forefoot, Achilles tendon, or subtalar joint. After a brief period of walking, the pain usually subsides, but returns again either with vigorous activity or prolonged standing or walking. On the field, an altered gait or abnormal stride pattern, along with pain during running or jumping activities are tell-tale signs of plantar fasciitis and should be given prompt attention. Further indications of the injury include poor dorsiflexion (lifting the forefoot off the ground) due to a shortened gastroc complex, (muscles of the calf). Crouching in a full squat position with the sole of the foot flat on the ground can be used as a test, as pain will preclude it for the athlete suffering from plantar fasciitis, causing an elevation of the heel due to tension in the gastroc complex.
Diagnosis
In more difficult cases of plantar fasciitis you should see your foot health professional for a thorough examination. They will find out why your arch or heel pain occurred in the first place and devise a treatment plan to relieve your pain and prevent it from reoccurring. They will evaluate your feet, walking pattern (gait), shoes, activities, exercise methods, and other relevant information and then devise your treatment plan.
Non Surgical Treatment
In addition to relieving the pain by providing better metatarsal support for your feet, many doctors advise stretching and strengthening the muscles that surround the damaged or weakened tendons. This advice can prove especially effective in preventing the possible side effects of fallen arches, including: inflammation and discomfort in the ligaments of the sole, Achilles tendonitis, shin splints, calluses, and bunions. Like plantar fasciitis, left untreated, fallen arches can cause a domino effect that impacts your legs, hips, and back.

Surgical Treatment
There are two types of bone procedure for flat feet, those where bone cuts and bone grafts are used to alter the alignment by avoiding any joint structures, or joint invasive procedures (called fusions or arthrodeses) that remove a joint to reshape the foot. With joint fusion procedures, there are those procedures that involve non-essential joints of the foot versus those that involve essential joints. All bone procedures have their place in flat foot surgery, and Dr. Blitz carefully evaluates each foot to preserve as much motion and function while obtaining proper and adequate alignment. In many cases a flat foot reconstruction involves both soft tissue procedures and bone procedures to rebuild and restore the arch. There are several joints in the arch of the foot that can collapse - and these joints are non-essential joints of the foot. This does not mean that they do not have a purpose, but rather become inefficient is providing a stable platform for function. As such, locking these non-essential non-functioning joints into place is commonly recommended. These joints are fused together with screws and/or plates. A heel bone that is no longer in proper position and pushed outwards away from the foot can be corrected with a bone cut and realignment procedure, so long as the displacement is not too significant. A benefit of this surgery is that it keeps the back portion of the foot mobile, and helps the surrounding tendons work for efficiently in maintaining the arch. In certain flat feet, the foot is deviated outwards and away from the midline of the body. Sometimes, this is due to the outer portion of the foot being shorter than the inner portion. Here bone graft can be added to the outer edge of the foot to lengthen the foot to swing the foot over into a corrected position. This procedure is most commonly performed in children and young adults. A bone graft is inserted into the top part of the arch to realign a component of the flat foot, medically known as forefoot varus or medial column elevatus. The back part of the foot (called the rearfoot complex) can be the cause (or source) of the flat foot or the simply affected by the flat foot foot. In simple terms, the back part of the foot can be made to flatten out due to arch problems - and vica versa for that matter. Dr. Blitz specifically identifies the cause of the flat foot as this will determine the best treatment plan, as each flat foot needs to be evaluated individually. The rearfoot is made up of three joints, and depending on the extent and most importantly the rigidity of these joints, they may require fusion to restore alignment. When all three joints require fusion - this call is a triple arthrodesis. For completeness, isolated fusion of any of the three joints can be performed (such as subtalar joint arthrodesis, talonavicular arthrodesis, and calcaneaocuboid joint arthrodesis). The medical decision making for isolated fusions is beyond the scope this article, but Dr. Blitz tries to avoid any rearfoot fusion for flexible feet because these are joints are essential joints of the foot, especially in younger people. Those in severe cases, it may be advantageous to provide re-alignment.
Prevention
Maintain a healthy weight, Use insoles to support your arches, Limit how often you wear high heels, Use proper shoes, especially when exercising to evenly distribute weight through your foot.
Stretching Exercises
Strength training and stretching can help avoid injury and keep your feet free from pain. Stretching should focus on the bottom of your foot to loosen tissues and tight ligaments surrounding your arch. The easiest way to do this is by grabbing a towel and sitting on the floor. You can do this while you catch up on the news in the morning, or when you get home from work. Put one leg out in front with your foot flexed up. Loop the towel around the ball of your foot and gently pull your toes towards you. Hold for thirty seconds and then repeat 3-4 times before switching feet.
Achilles Tendon Tear Treatments
Overview  A torn or ruptured Achilles tendon is simply no fun at all. This essential cord of strong, fibrous material attaches the heel bone to the calf muscles and is used in just about every movement, from walking and running to jumping and standing on your tip-toes. It also helps bend the foot downwards at the ankle. As the strongest tendon in the body, the Achilles can withstand a force of about 1,000 pounds. About 7 out of every 100,000 people will suffer from a ruptured Achilles at some point in time, with over 80% of these injuries occurring during a recreational sports activity. Athletes have a 24% chance of tearing their Achilles, but competitive runners have a 40 to 50% chance of Achilles tendon rupture during their lifetime. Causes Repeated stress from a variety of causes is often the cause of Achilles tendon injury. The stress may occur from any of the following. Excessive activity or overuse. Flat feet. Poorly fitting or inadequate shoes. Inadequate warm-up or proper conditioning. Jogging or running on hard surfaces. Older recreational athlete. Previous Achilles tendon injury (tendonitis/rupture). Repeated steroid injections. Sudden changes in intensity of exercise. Use of fluoroquinolone antibiotics (especially in children). Trauma to the ankle. Tense calf muscles prior to exercise. Weak calf muscles. Symptoms A sudden and severe pain may be felt at the back of the ankle or calf, often described as "being hit by a rock or shot" or "like someone stepped onto the back of my ankle." The sound of a loud pop or snap may be reported. A gap or depression may be felt and seen in the tendon about 2 inches above the heel bone. Initial pain, swelling, and stiffness may be followed by bruising and weakness. The pain may decrease quickly, and smaller tendons may retain the ability to point the toes. Without the Achilles tendon, though, this would be very difficult. Standing on tiptoe and pushing off when walking will be impossible. A complete tear is more common than a partial tear. Diagnosis A doctor will look at the type of physical activity you have been doing. He or she will then look at your foot, ankle and leg. An MRI may also be used. This is to help determine the severity of the tear and the extent of separation of the fibers. Non Surgical Treatment Not every torn Achilles tendon needs an operation. Recent studies have shown that even a conservative treatment, i.e. immobilizingt the leg can lead to satisfactory healing successes. This requires, however, that the patient is fitted with a cast (immobilization splint) and/or a special boot for a period of approximately 6 - 8 weeks. After that, the boot must be worn during the day for about two more weeks. An intensive physiotherapy will start after about six weeks to train the calf muscles so that the initial coordination can be restored. Running training on flat ground can be started again after another 10 - 12 weeks. Studies show that the danger of a recurring torn tendon is higher after a conservative treatment opposed to an operative treatment. Depending on the type of treatment, about 10 - 15 percent of those affected can expect at some point to again suffer from a tear of the Achilles tendon. Moreover, in the non-operated cases, we see more often a significant permanent weakness of the footprint, particularly restricting the ability to participate in sports.
A torn or ruptured Achilles tendon is simply no fun at all. This essential cord of strong, fibrous material attaches the heel bone to the calf muscles and is used in just about every movement, from walking and running to jumping and standing on your tip-toes. It also helps bend the foot downwards at the ankle. As the strongest tendon in the body, the Achilles can withstand a force of about 1,000 pounds. About 7 out of every 100,000 people will suffer from a ruptured Achilles at some point in time, with over 80% of these injuries occurring during a recreational sports activity. Athletes have a 24% chance of tearing their Achilles, but competitive runners have a 40 to 50% chance of Achilles tendon rupture during their lifetime. Causes Repeated stress from a variety of causes is often the cause of Achilles tendon injury. The stress may occur from any of the following. Excessive activity or overuse. Flat feet. Poorly fitting or inadequate shoes. Inadequate warm-up or proper conditioning. Jogging or running on hard surfaces. Older recreational athlete. Previous Achilles tendon injury (tendonitis/rupture). Repeated steroid injections. Sudden changes in intensity of exercise. Use of fluoroquinolone antibiotics (especially in children). Trauma to the ankle. Tense calf muscles prior to exercise. Weak calf muscles. Symptoms A sudden and severe pain may be felt at the back of the ankle or calf, often described as "being hit by a rock or shot" or "like someone stepped onto the back of my ankle." The sound of a loud pop or snap may be reported. A gap or depression may be felt and seen in the tendon about 2 inches above the heel bone. Initial pain, swelling, and stiffness may be followed by bruising and weakness. The pain may decrease quickly, and smaller tendons may retain the ability to point the toes. Without the Achilles tendon, though, this would be very difficult. Standing on tiptoe and pushing off when walking will be impossible. A complete tear is more common than a partial tear. Diagnosis A doctor will look at the type of physical activity you have been doing. He or she will then look at your foot, ankle and leg. An MRI may also be used. This is to help determine the severity of the tear and the extent of separation of the fibers. Non Surgical Treatment Not every torn Achilles tendon needs an operation. Recent studies have shown that even a conservative treatment, i.e. immobilizingt the leg can lead to satisfactory healing successes. This requires, however, that the patient is fitted with a cast (immobilization splint) and/or a special boot for a period of approximately 6 - 8 weeks. After that, the boot must be worn during the day for about two more weeks. An intensive physiotherapy will start after about six weeks to train the calf muscles so that the initial coordination can be restored. Running training on flat ground can be started again after another 10 - 12 weeks. Studies show that the danger of a recurring torn tendon is higher after a conservative treatment opposed to an operative treatment. Depending on the type of treatment, about 10 - 15 percent of those affected can expect at some point to again suffer from a tear of the Achilles tendon. Moreover, in the non-operated cases, we see more often a significant permanent weakness of the footprint, particularly restricting the ability to participate in sports.  Surgical Treatment Referral to a surgeon for open or percutaneous repair of the tendon is often necessary, followed by an immobilisation period. Functional bracing and early mobilisation are becoming more widely used postoperatively. There is no definitive protocol for this and it may differ, depending on the surgeon. Operative treatment has a reduced chance of re-rupture compared with conservative treatment (3.5% versus 12.6%) and a higher percentage of patients returning to the same level of sporting activity (57% versus 29%). The patient's desired functional outcome and comorbidities that affect healing will be factors in the decision to operate.
Surgical Treatment Referral to a surgeon for open or percutaneous repair of the tendon is often necessary, followed by an immobilisation period. Functional bracing and early mobilisation are becoming more widely used postoperatively. There is no definitive protocol for this and it may differ, depending on the surgeon. Operative treatment has a reduced chance of re-rupture compared with conservative treatment (3.5% versus 12.6%) and a higher percentage of patients returning to the same level of sporting activity (57% versus 29%). The patient's desired functional outcome and comorbidities that affect healing will be factors in the decision to operate.
Pes Planus?

There are many different causes of and treatments for flat foot. The most important part of treatment is determining the exact flat foot type on an individual basis, and doing so early on. The main objective is to become educated on the potential problems, so that you can stop them before they start. Conservative treatment is often successful if initiated early. The old adage "a stitch in time saves nine" definitely applies to the human body, hopefully more figuratively than literally. Do not ignore what your common sense and your body are telling you. Yes, you can live without an arch, but never neglect a symptomatic foot. If you neglect your feet, they will make you pay with every literal step you take.
Causes
The most common acquired flat foot in adults is due to Posterior Tibial Tendon Dysfunction. This develops with repetitive stress on the main supporting tendon of the arch over a long period of time. As the body ages, ligaments and muscles can weaken, leaving the job of supporting the arch all to this tendon. The tendon cannot hold all the weight for long, and it gradually gives out, leading to a progressively lower arch. This form of flat foot is often accompanied by pain radiating behind the ankle, consistent with the course of the posterior tibial tendon. Compounding matters is the fact that the human foot was not originally designed to withstand the types of terrain and forces it is subjected to today. Nowhere in nature do you see the flat hard surfaces that we so commonly walk on in present times. Walking on this type of surface continuously puts unnatural stress on the arch. The fact that the average American is overweight does not help the arch much either-obesity is a leading cause of flat feet as the arch collapses under the excessive bodyweight. Furthermore, the average life span has increased dramatically in the last century, meaning that not only does the arch deal with heavy weight on hard flat ground, but also must now do so for longer periods of time. These are all reasons to take extra care of our feet now in order to prevent problems later.
Symptoms
A significant number of people with fallen arches (flat feet) experience no pain and have no problems. Some, however, may experience pain in their feet, especially when the connecting ligaments and muscles are strained. The leg joints may also be affected, resulting in pain. If the ankles turn inwards because of flat feet the most likely affected areas will be the feet, ankles and knees. Some people have flat feet because of a developmental fault during childhood, while others may find that the problem develops as they age, or after a pregnancy. There are some simple devices which may prevent the complications of flat feet.
Diagnosis
You can always give yourself the ?wet test? described above to see whether you have flat feet. Most people who do not notice their flat feet or have no pain associated with them do not think to see a foot doctor. Flat feet can lead to additional problems such as stiffness or pain, however, especially if the condition appears out of nowhere. If you think you may have flat feet, you should seek medical attention to ensure there are no additional issues to worry about. Your doctor will be able to diagnose you with a number of tests. For example, he or she may have you walk around, stand still, or stand on your tiptoes while you are being examined. Your doctor may also examine your foot?s shape and functionality. It?s important to let your foot doctor know about your medical and family history. In some cases, your doctor may order imaging tests such as x-rays or an MRI (magnetic resonance imaging) to determine a cause of your flat foot. If tarsal coalition is suspected in children, a CT scan is often ordered.
Non Surgical Treatment
Switch activities for a little while. If you?re a super athlete, you don?t want to hear that you need to take a break, but there?s no way around it. You need to lay off the high impact sports like basketball, tennis and running. Don?t panic-there?s no shortage of alternatives. Find a high school track that?s open to the public and try going for a run. Many athletic programs use spongy synthetic materials to pave tracks instead of concrete. This is much easier on all the joints and tendons, not only in your feet but your legs and ankles. You can also try running on dirt trails or stable grassy areas. Take up swimming for a little while. This is actually an ideal activity for your arches. The buoyancy of water takes weight off our feet, but still allows for aerobic activity. Many gyms and activity centers also offer various water sport classes. In no time flat, you?ll be on your way to healthier feet.
Surgical Treatment

In cases of flat feet that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required and in some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you.
Prevention
Strap the arches into the anatomically correct positions with athletic tape and leave them like this for some time. If the fallen arches are an issue with the muscular structure, this may give the muscles an opportunity to strengthen. This is definitely not a fallen arches cure all the time but it can help prevent it more times than not. Ask a doctor or physical therapists to show you how to do this taping. Find shoes that fit. This may require that you get your foot measured and molded to ensure that the shoe will fit. Shoes that are too big, too tight or too short, may not directly cause the fallen arches, but they can assist with the damage to the area. These shoes should have thick cushioning inside and have plenty of room for your toes. Walk without shoes as much as possible. Shoes directly assist with weakening and distorting the arches of the feet so going without shoes can actually help strengthen your arches and prevent fallen arches. Walking on hard and bumpy surfaces barefooted makes the muscles in your feet strengthen in order to prevent injury. It is a coping mechanism by your body. Insert heel cups or insoles into the shoes that you wear the most. Many people wear uncomfortable shoes to work and these are the same shoes that cause their arches the most problems. Inserting the heel cups and insoles into these shoes can prevent fallen arches from occurring. Many people place these inserts into all their shoes to ensure support. Ask a medical professional, either your doctor or a physical therapist, about daily foot exercises that may keep the arches stronger than normal. Many times, you can find exercises and stretches on the Internet on various websites. Curling your toes tightly and rotating your feet will help strengthen your longitudinal arches. Relax your feet and shake them for a minute or so before you do any arch exercises. This will loosen the muscles in your feet that stay tight due to normal daily activities. Wear rigid soled sandals whenever possible to provide a strong support for your arches. Wooden soled sandals are the best ones if available. Walk or jog on concrete as much as you can. This will create a sturdy support for your arches. Running or walking in sandy areas or even on a treadmill, does not give rigid support. Instead, these surfaces absorb the step, offering no support for arches.